Medicare’s traditional “fee for service” (FFS) program is administered through several private health care companies that are each awarded a geographic jurisdiction which covers many different states that are not necessarily contiguous. These private companies are called Medicare Administrative Contractors (MACs). I live in Texas, so my MAC is Novitas.
If Medicare has issued a National Coverage Determination (NCD), then the MACs are not supposed to create policies that restrict national coverage. However, the MACs are allowed to create what are called Local Coverage Determinations (LCDs) to define the details of how they will implement Medicare policies. I’ve been watching policies relating to wound care and hyperbaric medicine for more than three decades, and it’s possible to see trends over that period of time.
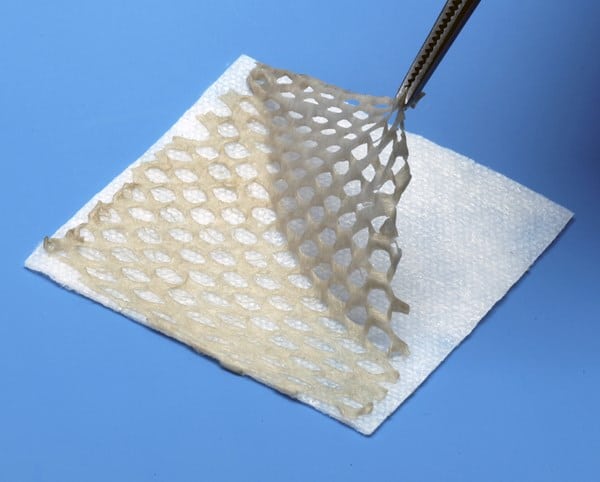
Novitas has issued a “new” LCD pertaining to the use of “skin substitutes” (more accurately called cellular and/or tissue-based products (CTPs)) for the treatment of Diabetic Foot Ulcers (DFUs) and Venous Leg Ulcers (VLUs). I am not even going to try to provide a comprehensive review of the details of the Novitas LCD, which is more of an update of previous policies. This is more a philosophical commentary about what’s going on.
You already know that the recently released Medicare Physician Fee Schedule (MPFS) proposed rule would, if implemented, make dramatic changes to the way that cellular and/or tissue-based products (CTPs) are covered in the physician’s office setting. Some people think that Medicare’s proposed changes to physician payment for CTPs is what emboldened the MACs to write more restrictive LCDs. However, given the timing, I think it’s more likely that the administrators at the Centers for Medicare and Medicaid Services (CMS) have been in conversation with the leadership of the various MACs for a long time about this topic. It feels planned to me. Once upon a time, it was common to see wide variations in regional MAC policies — but not any longer. LCDs for different regions (administered by different private companies) now often read like they just hit “copy and paste” from one LCD to another. Different LCDs even include the same inaccuracies, and none of them appear to be following the requirements of the “21st Century Cures” Act for the development of LCDs. Now it even appears that the regional Medicare contractors know in advance what CMS is going to do with payment policy.
My point is this: CMS (the mother ship in Baltimore), perhaps in collaboration with at least some of the regional MACs, have decided to curtail the use of “skin substitutes” by every possible method. CMS and the MACs have different types of authority. CMS can make sweeping changes to how they are reimbursed. The MACs can decide when they are reimbursed. CMS also decides what services to target for the alphabet soup of Medicare audits. They are also auditing claims for CTPs. The full attention of every aspect of CMS is now focused on the use of CTPs. Why do you think that is?