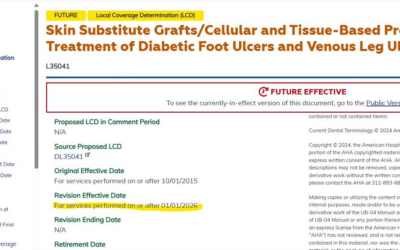
Novitas has issued a draft Local Coverage Determination (LCD) for the use of “skin substitutes” (more accurately known as Cellular and/or Tissue Based Products or CTPs) when used for treating Diabetic Foot Ulcers (DFUs) and Venous Leg Ulcers (VLUs). The proposed LCD has been posted to Novitas’ website for comments.
This is Part 4 of the list of what you need to document (per the proposed rule) if you want to use a skin substitute (CTP) for a DFU or VLU.
I am pointing out just a few interesting and important things about the way that documentation impacts coverage for CTPs in these two types of chronic ulcerations – based on the proposed rule.
I mentioned last time that the most intriguing part of the proposed policy is the list of what is NOT considered “medically reasonable and necessary”. The first of the list is that Novitas does not consider it medically necessary to apply “greater than two applications of a specific skin substitute graft product within the episode of skin replacement surgery for wound care (defined as 12 weeks from the first application of a skin substitute graft).”
Here’s more of the list of what is “not medically necessary” with regard to CTP applications in the proposed rule (I have put my comment in italics):
- Treatment will consist of “the fewest repeat applications” to heal the wound
- They already set the limit at 2 so this is confusing
- [treatment will consist of the least] amount of product to heal the wound.
- Later it goes on to say the following about “Excessive wastage (discarded amount).” “The skin substitute graft must . . .[utilize] the smallest package size available for purchase from the manufacturer that could provide the appropriate amount for the patient.
- Pay attention to that one because it’s a huge problem in the hospital-based outpatient department (HOPD). Most HOPDs are limited with regard to the size of product used and besides that, the products are under “package pricing” so Medicare is reimbursing every product at the same rate no matter what size it is. This was clearly put into the policy because a doctor’s office can get reimbursed for the total cost of the product and thus using a larger product than needed will waste Medicare dollars.
- The point is that if you put on a product that is larger than the wound, you had better explain why.
- Later it goes on to say the following about “Excessive wastage (discarded amount).” “The skin substitute graft must . . .[utilize] the smallest package size available for purchase from the manufacturer that could provide the appropriate amount for the patient.
- “Switching skin substitute graft products in a 12-week episode of skin replacement surgery for wound care.”
- Exceptions may be “considered on appeal.” Good luck.
- “Application of a skin substitute graft product beyond 12-weeks.”
- “Repeat applications of skin substitute grafts when a previous application was unsuccessful.”
- “Unsuccessful treatment is defined as increase in size or depth of an ulcer, or no change in baseline size or depth and no sign of improvement or indication that improvement is likely (such as granulation, epithelialization, or progress towards closing).”
- Surgical preparation services (for example, debridement), in conjunction with . . . skin replacement surgery
- All liquid skin substitute products for wound care
Believe it or not, there’s still more to come.
If you want to present comments on any part of Novitas proposed LCD, sign up to attend the Open Meeting. Register by the August 24th deadline using the appropriate presenter or observer registration link.