The MACs (Medicare Administrative Contractors) have been auditing wound debridements. I thought it might be useful to understand the history of debridement audits. But first we should start with WHY Medicare is auditing charges in the traditional “fee for service” part of Medicare. The Alliance of Wound Care Stakeholders published what is perhaps the best a study on the cost of wound care for Medicare beneficiaries, using 2014 Medicare claims data. One of the many interesting discoveries was that the largest portion of Medicare costs for wound care occur in the outpatient setting. This surprised nearly everyone but wound care practitioners. (The paper was published open source so that a complete copy is available to you at this link.)
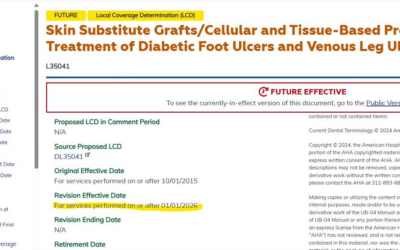
I’m looking at this today through the lens of debridement because of the Novitas Local Coverage Determination (LCD) on Wound Care. (Novitas is my MAC because I am in Texas.)
The Novitas LCD states:
“…only a minority of beneficiaries who undergo debridements for wound care appear to require more than eight total surgical excisional debridement services involving subcutaneous tissue, muscle/fascia, or bone in a 360 day period, (five debridements of which involve removal of muscle/fascia, and/or bone).”
A history lesson is useful to understand how we got here. Let’s go back in time a decade from the 2014 data used for the Value in Health project, all the way back to 2004 when the Office of the Inspector General (OIG) performed an audit of debridement services. You can find a copy using this link: Medicare Payments for Surgical Debridement Services in 2004 (PDF)
The OIG performed this audit because it had seen a dramatic increase in the number of Medicare claims submitted for the surgical debridement of wounds under CPT codes 11040 – 11044 (the codes have changed somewhat since then). In 2004, Medicare paid out $188 million for surgical debridement services. Here’s what the OIG said in their report, published in 2007:
- 64% of surgical debridement services did not meet Medicare program requirements
- 47% of miscoded services were not actually surgical debridements
- 20% of services billed as a debridement were actually routine foot care (e.g. removal of a callus)
- 29% were either not documented at all, or insufficiently documented so that there wasn’t enough information to even determine whether the services were medically necessary or coded correctly
The OIG also concluded that some of these services might even have been part of an “inappropriate pattern.” For example, one patient had 43 debridement’s involving muscle within a 9-month period. If you are wondering why Novitas would attempt to limit or at least curtail the number of debridements performed per patient, per year, it’s because of clinicians like this person.
In 2004, the OIG recommended that the Center for Medicare and Medicaid Services (CMS) strengthen program safeguards to “prevent improper payments” for surgical debridement services. They specifically recommended:
- CMS should instruct the carriers to conduct additional medical reviews and education efforts on surgical debridement services AND
- CMS should either develop a National Coverage Determination or instruct carriers to develop more uniform policy guidance, such as an LCD (italics mine)
After that, TrailBlazer Health Enterprises, the carrier and fiscal intermediary for Medicare in Texas back then (before Novitas), performed probe audits on wound debridements and they, too found a lack of documentation to support the medical necessity of the debridement procedures as billed. In 2007, Trailblazer issued an LCD that limited the number of debridements involving muscle and/or bone to fewer than 5 per year.
In 2010, RAC auditors began to hit hard on debridement documentation, looking for 5 elements: technique used, instruments used, tissue removed, appearance and size of wound, and depth of debridement performed.
In 2011, RAC auditors started looking at improperly billed debridement services billed by hospitals (e.g. services being billed as surgical debridements that were not).
It’s important to pay attention to the sequence of events:
- Claims data show a spike in billed services for a code or group of codes
- The OIG performs an audit and finds worrisome issues pertaining to documentation and/or compliance with Medicare policy
- The MAC issues an LCD to address compliance with coverage policy and limit inappropriate use or over-use
- RAC auditors begin recovery audits
In the case of debridement charges, this process began in 2004 with the OIG audit (published in 2007) and RAC recovery beginning around 2010. It is now 2017. The OIG report on debridement services was published a decade ago, and RAC audits of debridement charges have been going on in various places for many years. The Novitas LCD language around debridement is similar to that enacted by Trailblazer ten years ago.
How do these threads tie together? The cost of wound care is staggering, and outpatient wound care services comprise the largest portion of spending. The OIG found evidence of improper billing of debridements years ago, and RAC auditors are recouping money from debridement services. In light of these facts, it is simply not possible for either hospital wound centers or wound care clinicians to use repetitive debridement charges as an engine with which to power their revenue train. The danger of doing so has been widely known for a decade. And if you have a written policy that patients will undergo “weekly debridements,” you could be in for a lot of pain when the auditors come for you.